Duodenal Switch
Home -> Duodenal Switch
- Laparoscopic Sleeve Gastrectomy
- Roux-en-Y Gastric Bypass Surgery
- Mini Gastric Bypass
- Endoscopic Sleeve Gastroplasty
- Single Anastomosis Duodenal Switch
- Duodenal Switch
- Revisions Surgeries
Overview
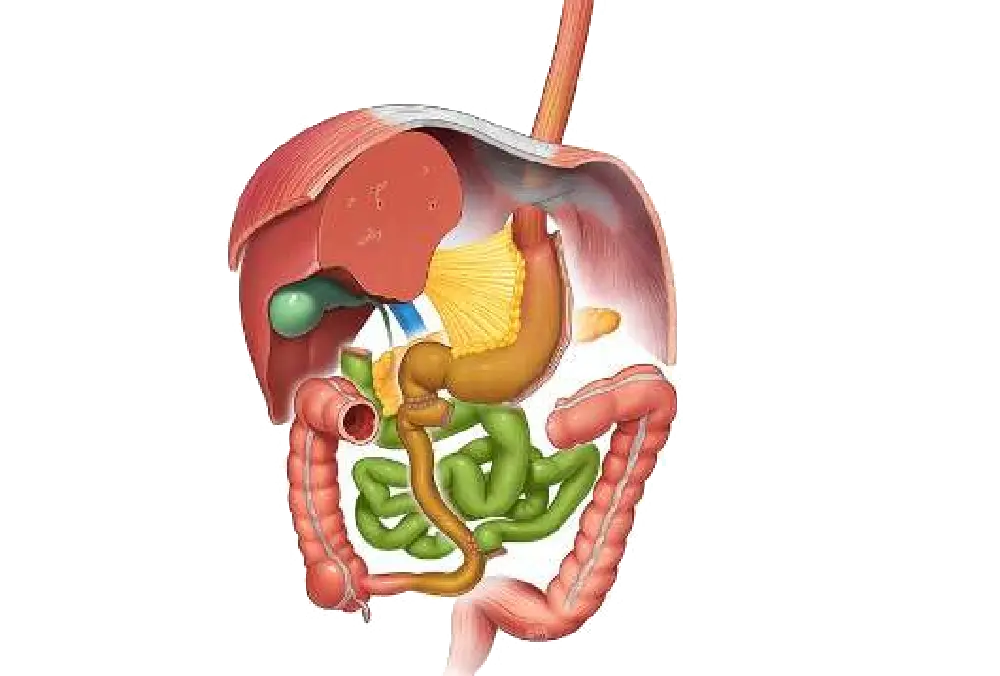
The Duodenal Switch (DS) is a powerful and highly effective weight-loss surgery that combines two procedures: a gastric sleeve and an intestinal bypass.
Known for its ability to achieve significant and sustained weight loss, the duodenal switch is often recommended for patients with severe obesity and obesity-related health conditions.
How Does Duodenal Switch Work?
- Gastric Sleeve:
The first step of the duodenal switch involves the removal of a large portion of the stomach, leaving behind a sleeve-shaped stomach that limits the amount of food you can consume. This reduces hunger and helps with portion control. - Intestinal Bypass:
The small intestine is rerouted so that food bypasses a large portion of the stomach and the upper part of the small intestine (duodenum). This limits the absorption of calories and nutrients, resulting in significant weight loss. - Malabsorption:
The rerouting of the intestine reduces the absorption of calories and fat from food, contributing to faster weight loss and improved blood sugar levels in patients with type 2 diabetes.
Benefits of Duodenal Switch
- High Weight Loss:
Duodenal Switch leads to substantial weight loss, with patients typically losing 70-80% of their excess weight within 12-18 months after surgery. - Improvement in Health Conditions:
This procedure can improve or resolve conditions like type 2 diabetes, sleep apnea, high blood pressure, and fatty liver disease. - Sustained Results:
The combination of restriction and malabsorption makes the duodenal switch one of the most effective long-term weight-loss surgeries. - Better Control Over Hunger:
The gastric sleeve component reduces hunger hormones, helping patients control their food intake effectively.
Who is a Good Candidate for Duodenal Switch?
Duodenal Switch is ideal for individuals who:
- Have a BMI of 40 or higher or a BMI of 35 or higher with obesity-related health conditions.
- Have been unsuccessful with diet and exercise alone.
- Are committed to making long-term lifestyle changes.
- Need significant weight loss to improve health and quality of life.
Risks and Considerations
- Nutritional Deficiencies:
Since the surgery reduces the absorption of nutrients, patients need to take lifelong vitamins and mineral supplements to avoid deficiencies. - Complexity:
The procedure is more complex than other weight-loss surgeries and requires a longer hospital stay and recovery period. - Potential for Complications:
While rare, complications such as bowel obstructions, leaks, or infections may occur. - Lifestyle Commitment:
Patients must commit to a healthy diet and regular physical activity, along with regular follow-up visits to monitor their progress.
Conclusion
The Duodenal Switch (DS) offers one of the most effective weight-loss surgeries for individuals with severe obesity. Its combination of restricting food intake and bypassing part of the small intestine leads to rapid and sustained weight loss. However, it requires lifelong dedication to diet, supplementation, and regular check-ups to maintain optimal health and avoid complications.